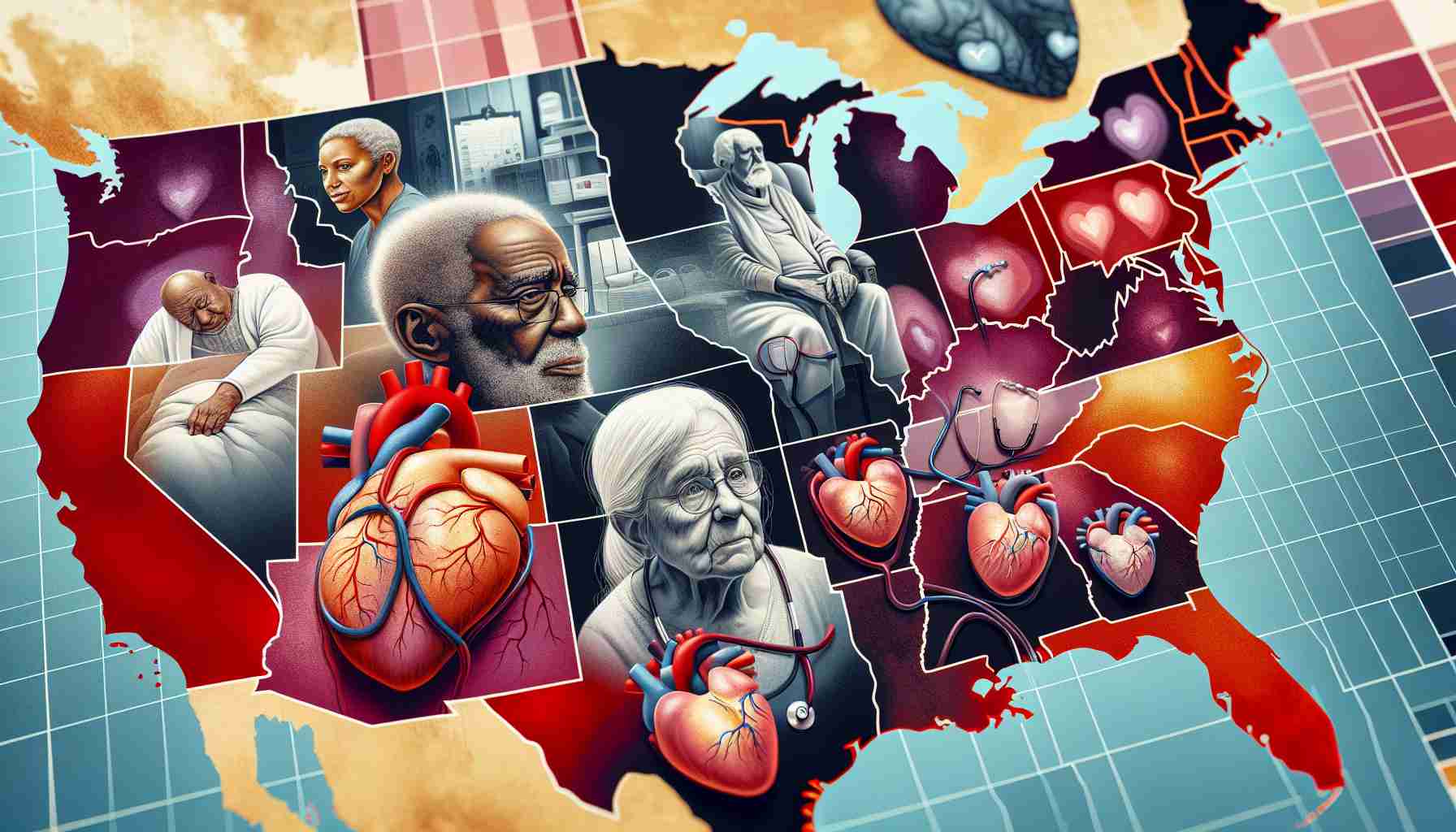
A recent investigation sheds light on the unequal provision of palliative care services for individuals diagnosed with heart failure in the United States. Despite recommendations from prominent medical associations regarding the integration of palliative care into heart failure management, there remains a substantial gap in practice.
The study, brought to attention in a reputable cardiovascular journal, uncovered that only a fraction of heart failure patients, approximately one in eight, receive palliative care consultations within five years of diagnosis. This figure starkly contrasts with the level of palliative care access observed in patients with terminal cancers, revealing a concerning disparity in healthcare provision.
Moreover, the research highlighted noteworthy racial and regional discrepancies, indicating that Black individuals are notably less likely to receive palliative care compared to their white counterparts. This trend is particularly troubling given the heightened risk and mortality rates associated with cardiovascular disease in the Black community.
The primary researcher behind this study, Zidong Zhang, emphasized the urgent need for systemic reforms to facilitate early integration of palliative care for heart failure patients. By addressing payment system barriers, enhancing physician guidance on palliative care initiation, and expanding community-based services, the healthcare system can strive towards achieving equitable access to critical end-of-life care for all individuals with heart failure.
Exploring Further Disparities in Palliative Care Access for Heart Failure Patients
A deeper examination of the disparities in palliative care access for individuals with heart failure in the United States unveils additional critical insights beyond what has been previously outlined. While the existing investigation sheds light on the overall lack of palliative care provision, further research reveals nuanced factors contributing to this gap.
Key Questions and Answers:
1. What are the contributing factors to the disparities in palliative care access for heart failure patients?
Several factors contribute to these disparities, including inadequate training among healthcare providers in identifying the need for palliative care, misconceptions about palliative care as solely end-of-life care rather than a holistic approach, and financial barriers hindering access to these services.
2. How do disparities in access to palliative care impact patient outcomes?
Disparities in access to palliative care can result in increased symptom burden, higher rates of hospital readmissions, and reduced quality of life for heart failure patients. Without timely access to supportive care, patients may experience unnecessary suffering and a lack of coordination in their treatment plans.
Key Challenges and Controversies:
One of the significant challenges in addressing these disparities lies in changing the perception of palliative care among patients, families, and healthcare providers. Overcoming the stigma associated with palliative care as solely end-of-life care is crucial to promoting its integration as an essential component of heart failure management.
Advantages and Disadvantages:
Advantages:
– Early integration of palliative care can improve symptom management, enhance patient satisfaction, and facilitate shared decision-making between patients, families, and healthcare providers.
– Palliative care can improve the overall quality of life for heart failure patients by addressing physical, emotional, and spiritual needs throughout the course of the disease.
Disadvantages:
– Limited awareness and education about palliative care may lead to underutilization of these services, resulting in unmet needs and increased healthcare costs associated with avoidable hospitalizations.
– Establishing equitable access to palliative care requires systemic changes in healthcare delivery, reimbursement models, and training programs, which may pose financial and logistical challenges.
For more information and resources on disparities in healthcare access, you can explore reputable organizations such as the National Institutes of Health or the Centers for Disease Control and Prevention. These institutions provide valuable insights and research findings on improving access to palliative care and reducing disparities in healthcare provision across diverse patient populations.